Cataracts
 Your eye works a lot like a camera. Light rays focus through your lens onto the retina, a layer of light-sensitive cells at the back of the eye. Similar to photographic film, the retina allows the image to be “seen” by the brain.
Your eye works a lot like a camera. Light rays focus through your lens onto the retina, a layer of light-sensitive cells at the back of the eye. Similar to photographic film, the retina allows the image to be “seen” by the brain.
Over time, the lens of our eye can become cloudy, preventing light rays from passing clearly through the lens. The loss of transparency may be so mild that vision is barely affected, or it can be so severe that no shapes or movements are seen – only light and dark. When the lens becomes cloudy enough to obstruct vision to any significant degree, it is called a cataract. Eyeglasses or contact lenses can usually correct slight refractive errors caused by early cataracts, but they cannot sharpen your vision if a more advanced cataract is present.
The most common cause of cataract is aging. Other causes include trauma, medications such as steroids, systemic diseases such as diabetes, and prolonged exposure to ultraviolet light. Occasionally, babies are born with a cataract.
Cataracts typically develop slowly and progressively, causing a gradual and painless decrease in vision. Other changes you might experience include blurry vision; glare, particularly at night; frequent changes in your eyeglass prescription; a decrease in color intensity; a yellowing of images; and in rare cases, double vision.
As the eye’s natural lens gets harder, farsighted (hyperopic) people, who have difficulty focusing up close, can experience improved near vision and become less dependent on reading glasses. However, nearsighted (myopic) people become more nearsighted, causing a worsening in their distance vision. Some kinds of cataracts affect distance vision more than reading vision. Others affect reading vision more than distance vision.
Reducing your exposure to ultraviolet light by wearing a wide-brimmed hat and sunglasses may reduce your risk for developing a cataract, but once one has developed, there is no cure except to have the cataract surgically removed.
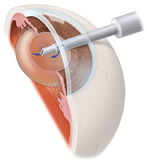 With a routine, outpatient surgical procedure, an ophthalmologist (Eye M.D.) can remove the cataract, making either a small incision (phacoemulsification) or a larger incision (extracapsular extraction). Usually, a synthetic intraocular lens (IOL) is inserted at the time of cataract extraction to replace the focusing power of the natural lens. IOL’s can be monovision (fixed-focus for a preset distance) or multifocal, which allows focused vision at many distances. The time to have cataract surgery is when the cataract is affecting your vision enough to interfere with your normal lifestyle.
With a routine, outpatient surgical procedure, an ophthalmologist (Eye M.D.) can remove the cataract, making either a small incision (phacoemulsification) or a larger incision (extracapsular extraction). Usually, a synthetic intraocular lens (IOL) is inserted at the time of cataract extraction to replace the focusing power of the natural lens. IOL’s can be monovision (fixed-focus for a preset distance) or multifocal, which allows focused vision at many distances. The time to have cataract surgery is when the cataract is affecting your vision enough to interfere with your normal lifestyle.
Cataract surgery is a very successful operation. One and a half million people have this procedure every year in the United States, and 95% have a successful result. As with any surgical procedure, complications can occur during or after surgery, and some are severe enough to limit vision. But in most cases, vision, as well as quality of life, improves.
What are cataracts?
Getting to know cataracts & astigmatism
Cataract surgery: the basics
Treating astigmatism & presbyopia during cataract surgery
Cataract Patient Counselor Complete
Cataract Patient Counselor LenSx® Laser
Cataract Patient Counselor ORA System® Technology
Cataract Patient Counselor Cataract Education
Toric IOL
 Current technology makes it possible to correct the cataracts that may be clouding your vision – and the astigmatism that may be distorting your vision – all at the same time.
Current technology makes it possible to correct the cataracts that may be clouding your vision – and the astigmatism that may be distorting your vision – all at the same time.
What is Astigmatism? Sometimes, the surface of the cornea is curved in such a way that vision becomes distorted or blurred. A person who has both cataracts and a corneal astigmatism will not regain high-quality distance vision after cataract surgery unless the astigmatism is also corrected.
What is the AcrySof® Toric IOL? The AcrySof® Toric intraocular lens (IOL) replaces your eye’s natural clouded lens during cataract surgery. It has the ability to reduce or eliminate corneal astigmatism at the same time it corrects cataracts. The result is typically improved distance vision, and less dependence on spectacles. However, most patients still need corrective lenses for near and intermediate tasks. The AcrySof Toric lens also filters out harmful ultraviolet and blue light.
With the AcrySof® Toric lens, your distance vision can be clear and vibrant, giving you the power to see your best and be your best.
AcrySof® IOLs are:
- The most widely used: More than 30 million have been implanted worldwide
- Unique in their ability to filter high-energy blue light
- Made by Alcon®, the world’s leading eye care company
Glaucoma
 Glaucoma is the leading cause of blindness and visual impairment in the United States. A simple painless eye exam can detect the disease. With early detection and treatment, glaucoma can usually be controlled and blindness prevented.
Glaucoma is the leading cause of blindness and visual impairment in the United States. A simple painless eye exam can detect the disease. With early detection and treatment, glaucoma can usually be controlled and blindness prevented.
Glaucoma can affect anyone from newborn infants to the elderly. It has been estimated that up to 3 million Americans have glaucoma. At least half of those people do not know they have it because glaucoma usually has no symptoms. People who are at a greater risk for glaucoma usually have the following conditions:
- At least 45 years old without regular eye exams
- A family history of glaucoma
- Abnormally high eye pressure
- African descent
- Nearsightedness
- Diabetes
- Previous eye injury
- Regular, long-term use of cortisone/steroid products
To detect glaucoma, your physician will test your visual acuity, examine the eyes and optic nerve and test the pressure in your eye. Regular and complete eye exams help to monitor the changes in your eyesight and will help to determine whether you may develop glaucoma.
Treatment to control glaucoma include medications in the form of either eyedrops or pills, laser surgery and conventional surgery.
Diabetes
Diabetic retinopathy is a potentially blinding complication of diabetes mellitus which causes abnormalities in the tiny blood vessels nourishing the retina. These blood vessels swell and leak blood damaging the retina, the light-sensitive tissue, which lines the back portion of the eye. Left untreated, diabetic retinopathy can result in severe loss of vision and ultimately blindness.
The causes of diabetic retinopathy are not certain, but it has been determined that the fluctuation in blood sugar levels leads to an increased risk of this disease, as well as long-term diabetes. There are two stages of diabetic retinopathy, nonproliferative, or background retinopathy, and proliferative retinopathy. In this early stage of nonproliferative retinopathy your symptons may include blurred or changing vision from the leaking blood that obscures the light sensitive retina. Proliferative retinopathy is the more advanced stage of this disease. New blood vessels grow abnormally in the retina and this growth can lead to scarring or retinal detachment which can lead to total blindness.
The location of the disease and the degree of damage to the retina determines the type of treatment of diabetic retinopathy. There are three effective methods in reducing vision loss from this disease. One method is to treat with laser photocoagulation, a way of sealing off the leaking blood vessels and removing new growth. The second treatment option involves intraocular medicines such as Avastin and triamcinolone (Kenalog). Another procedure is to perform conventional eye surgery, a vitrectomy, to remove blood that has leaked into the vitreous humor replacing it with a saline solution.
The best treatment for diabetic retinopathy is prevention. Early detection and management is important to prevent the development of the more sight damaging stages of the disease. Keeping your blood sugar at an even level and frequent eye examinations, as recommended by your physician, will help. With careful monitoring, treatment of diabetic retinopathy can be started before your sight is affected.
For more information about diabetic retinopathy, visit www.nei.nih.gov.
Dry Eye
 In order for your eyes to be comfortable and see well, a healthy tear film is required. If you are not producing the appropriate quality or quantity of tear film, you may be experiencing dry eye, also called ocular surface dysfunction.
In order for your eyes to be comfortable and see well, a healthy tear film is required. If you are not producing the appropriate quality or quantity of tear film, you may be experiencing dry eye, also called ocular surface dysfunction.
Symptoms of dry eye include burning, stinging, foreign body or sandy sensation, blurry vision, and stringy mucous. Sometimes people with dry eye can experience excess tearing as the eye reflexively responds to the dryness.
Dry eye symptoms increase as our eyes mature and tear quality and quantity change. Many women experience dry eye after menopause.
Treatments are varied but there is no cure. Artificial tears of various viscosities can provide relief and improve lubrication. In order to conserve your own tears, tiny plugs can be used to close the channels through which your tears drain. Restasis, a prescription drop, can increase your natural tear production when used regularly over time. Proper eyelid hygiene can also improve the health of the ocular surface. Other treatments are available and can be discussed with your ophthalmologist.
Activities causing prolonged staring such as reading, watching TV, and computer work can lead to tear film evaporation and dry eye symptoms. Wind, dust, smoke, and allergens can all aggravate the eye and worsen symptoms.
Pediatrics
 The brain cells that control vision are not fully developed at birth and the child’s eye also undergoes maturation throughout the first decade of life. Hence disorders that have little effect on adults may have a profound and life-long effect on a child’s vision. A pediatric ophthalmologist undergoes additional training and has experienced treating ocular disorders that may be unique to children, including eye muscle disorders (Strabismus) and lazy-eye (Amblyopia).
The brain cells that control vision are not fully developed at birth and the child’s eye also undergoes maturation throughout the first decade of life. Hence disorders that have little effect on adults may have a profound and life-long effect on a child’s vision. A pediatric ophthalmologist undergoes additional training and has experienced treating ocular disorders that may be unique to children, including eye muscle disorders (Strabismus) and lazy-eye (Amblyopia).
Strabismus is a medical term relating to misalignment of the eyes, either inward (“cross-eyed”) or outward (“wall-eyed”), or up or down. This largely occurs in children, perhaps apparent at birth or developing later either intermittently or associated with fatigue, illness, or near vision activities. There are numerous types and causes of strabismus for which there are different specific treatments ranging from eye exercise programs to advanced adjustable eye muscle surgery. Unless detected and treated, strabismus can result in amblyopia, a depression of vision in the deviant eye which may be permanent. Parental suspicion and immediate ophthalmologic diagnosis and treatment is imperative to prevent amblyopia and re-establish straight eyes.
Strabismus occurring for the first time in an adult is a common cause of intermittent or constant double vision. It may occur in an adult with a history of childhood strabismus or as a result of vascular insufficiency to a nerve that controls eye muscles. Although amblyopia cannot develop in an adult, the bothersome double vision commands prompt attention and a search for its cause.
